Table of Contents
- Overview
- What Is Plantar Fasciitis
- Plantar Fascia Pain
- What Is the Main Cause of Plantar Fasciitis?
- What Are the Risk Factors That Make It More Likely To Develop Plantar Fasciitis?
- What Can Be Mistaken for Plantar Fasciitis
- Ruptured Plantar Fascia
- What are some common conditions that mimic Plantar Fasciitis and how can they be distinguished?
- How Do You Treat Plantar Fasciitis?
- What Happens if You Don’t Treat Plantar Fasciitis
- Conclusion
- FAQ
Overview
Plantar Fasciitis (plan-tar fa-shee-aiy-tuhs) is one of the most common orthopedic complaints seen by Canadian Certified Pedorthists and a frequent cause of heel pain. It can be discouraging to experience heel pain day after day, so read on to inform yourself more thoroughly about this condition. This article will prepare you for a visit to your Pedorthist with an in-depth look at the symptoms, causes, diagnosis, and treatment of Plantar Fasciitis. It will also provide you with a brief overview of conditions that have similar symptoms to help you determine if Plantar Fasciitis is actually the cause of your pain.
What Is Plantar Fasciitis
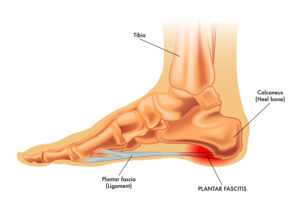
Your plantar fascia is the thick, web-like band of tissue that connects the front of your foot to your heel and supports the arch of your foot. This ligament experiences a lot of stress throughout your life, and when it begins to degenerate and/or becomes inflamed, the resulting condition is called Plantar Fasciitis (literally, inflammation of the plantar fascia).
Plantar Fasciitis is common. It affects about 10% of the general population at some point in their lives and accounts for approximately 80% of all heel pain complaints. For some people, Plantar Fasciitis is simply a nuisance that will resolve itself in a short period of time. For others, it can be chronically debilitating and even require surgical intervention.
Plantar Fascia Pain
Plantar Fasciitis is most classically associated with pain directly under the heel bone (calcaneus), but sometimes pain also manifests further forward under the arch of your foot. Pain from Plantar Fasciitis is typically worst when taking your first few steps in the morning or after a period of inactivity. It generally improves (though may not completely resolve) during gentle to moderate activity.
What Is the Main Cause of Plantar Fasciitis?

Although the cause remains unclear in some cases, most cases of Plantar Fasciitis occurs via stress to the plantar fascia. Such stress is most often due to stretching and overuse of the ligament, which results in tearing and inflammation. Sometimes, your lifestyle, habits, and natural physiology can make you more prone to Plantar Fasciitis.
What Are the Risk Factors That Make It More Likely To Develop Plantar Fasciitis?
- Tighter Calf Muscles Than Usual – Tight calf muscles make it difficult to flex your foot and bring your toes up towards your shin, which can increase the occurrence of Plantar Fasciitis.
- Obesity – Being overweight places extra stress on all parts of your body, including your feet and plantar fascia.
- Age – Most cases of Plantar Fasciitis occur in adults between the ages of 40 and 70 years old.
- Foot Type/Structure – Flat feet or very high arches can both impact the stress on your plantar fascia.
- Repetitive Impact Activities – Runners, dancers, and other high-impact athletes are at increased risk for heel pain due to Plantar Fasciitis.
- Occupations That Keep You on Your Feet – If you stand all day long, take measures to prevent Plantar Fasciitis. High-risk occupations include but are not limited to nurses, teachers, chefs, and cashiers.
- New or Increased Activity – Make sure you build up your strength and stamina gradually when starting a new active hobby or workout routine. Give your plantar fascia a chance to adjust and keep up!
What Can Be Mistaken for Plantar Fasciitis
Although Plantar Fasciitis is one of the most common causes of heel pain, there are plenty of other conditions with similar symptoms. The following list is intended to inform you about some such conditions, but it is always best to see your Pedorthist to discuss what is happening in your feet and legs.
Ruptured Plantar Fascia
If you already suffer from chronic Plantar Fasciitis or experienced recent trauma to your foot, you could have a ruptured plantar fascia. While the symptoms may be similar to those of Plantar Fasciitis, a plantar fascia rupture typically presents with more severe pain and may be accompanied by a sudden “pop” followed by swelling, bruising, and the inability to bear weight. A ruptured plantar fascia usually requires immediate medical intervention.
What are some common conditions that mimic Plantar Fasciitis and how can they be distinguished?

Arthritis
In many cases, Arthritis mimics Plantar Fasciitis very closely. Both conditions affect the heel joint, worsen when activity occurs after a period of rest, and subside when the joint is inactive. If Arthritis is suspected, your doctor will likely need to use diagnostic imaging to help determine the cause of your pain.
Stress Fracture
A calcaneal stress fracture (fracture of the heel bone) is another potential culprit of heel pain. This type of fracture is often found in people who do a lot of high-impact activity and/or have recently increased their activity level without first building up their strength and stamina. If your heel pain came on suddenly or was caused by trauma, suspect a stress fracture. The pain from stress fractures is usually more localized than the pain from Plantar Fasciitis and worsens with gentle activity instead of improving. Stress fractures are often diagnosed with an x-ray.
Circulatory Issues
Because your feet are the furthest extremities from your heart, the first symptoms of circulatory issues can sometimes be foot or heel pain. If your feet are often cold as well as painful, or if you have other symptoms such as varicose veins, or swelling in your legs or feet, it’s important to have a doctor rule out circulatory problems–even if you’re pretty certain the pain you’re experiencing is from Plantar Fasciitis. Proper precautions could be life-saving!
Nerve Entrapment
Nerve entrapment occurs when a nerve sends out a pain signal while being pinched by a structure such as a bone, muscle, or cyst. Often, this results in referred pain–where the pain is felt in a different location from where the actual entrapment is occurring. If the tibial nerve, which runs down the back of your leg, becomes entrapped near your ankle, this can result in heel pain. If your heel pain also involves tingling, or you can replicate it with your foot in the air (non-weight bearing), suspect nerve entrapment.
Sciatica
Another nerve condition that can result in referred pain in your heel or foot is Sciatica from a bulging or herniated disc in your spine. Like nerve entrapment, Sciatica can be distinguished from Plantar Fasciitis by the presence of tingling or numbness. It is also often associated with shooting pain up your leg.
Fat Pad Atrophy
Over time, the fat in your heel pad can begin to thin out or break down. This process reduces or eliminates the cushioning around your heel bone and can result in pain from bone bruising. Pain from an atrophied fat pad can closely mimic Plantar Fasciitis. A Pedorthist can examine your heel pad to determine whether or not its degeneration might be contributing to your pain.
Achilles Tendon Rupture
A ruptured Achilles Tendon is a severely painful injury that impacts the back of your heel more than the bottom (your Achilles tendon runs along the back of your ankle from your heel to your calf). While it may mimic Plantar Fasciitis in some ways, a ruptured Achilles Tendon is nearly always associated with severe trauma and an inability to bear weight.
Achilles Tendonitis
Tendonitis is very similar to Plantar Fasciitis but can occur in any tendon in the foot (or body). Tendonitis in your Achilles Tendon, which runs along the back of your ankle from your heel to your calf, is sometimes confused with Plantar Fasciitis but generally affects the back of the heel rather than the bottom.
Bursitis
Bursae throughout the body, including on the bottom of your feet, can become inflamed and painful due to repetitive stress. Unlike Plantar Fasciitis, Bursitis is associated with pain due to compression. If massaging or pressing on the sole of your foot/heel is sensitive and painful, the cause could be Bursitis.
How Do You Treat Plantar Fasciitis?

There is a range of treatment options for Plantar Fasciitis. In severe cases, surgical intervention may be warranted. But in most cases, conservative, non-invasive treatments are highly effective and can be used simultaneously to reduce symptoms and improve outcomes.
Non-Surgical Treatments
- Rest – It probably goes without saying, but rest is one of the most basic and important ways to heal your plantar fascia. Staying off your feet altogether may be impractical, but reducing your activity level and elevating your feet when possible are perfect ways to get your plantar fascia back on track.
- Ice – Ice reduces inflammation. Use it for 10 minutes on and 10 minutes off, especially after activity, to ease your symptoms.
- Taking Pain Relievers – Non-steroidal anti-inflammatories (NSAIDs) like ibuprofen or naproxen can temporarily relieve pain and reduce inflammation.
- Cortisone Injections – Your health care provider may also suggest a steroid injection as an option if your Plantar Fasciitis is severe and persistent.
- Supportive Shoes – High heels and other unsupportive footwear, like flip flops or soft soled shoes, are a major contributor to the development of Plantar Fasciitis. Your Pedorthist can treat your Plantar Fasciitis by fitting you with shoes that provide adequate support and cushioning for your lifestyle.
- Custom Made Foot Orthotics – A foot orthotic is a device that can be discreetly inserted into the shoe to support, align, prevent, and/or accommodate foot abnormalities and improve how the foot functions. After a thorough biomechanical assessment, your Canadian Certified pedorthist will discuss the type of orthotic that is best suited for your foot type and your lifestyle. There are many different materials that orthotics can be made from, and choosing the one best for you and your foot condition is very important. Canadian Certified Pedorthists are one of only 2 professionals who specialize in the manufacturing of custom made foot orthotics. You will always be casted using a 3 dimensional casting method which captures the shape and structure of your feet.
- Exercise – Ceasing all exercise is unhealthy and is not a recommended strategy for improving your Plantar Fasciitis. Modifying your exercise routine, however, will lower the impact on your plantar fascia and strengthen it for the future. One important element of your new routine will be proper stretching. Here are two stretches that, when done properly, are excellent for mitigating Plantar Fasciitis:
- Calf Stretch – With your toes pointing forward, put your hands on a wall and place one leg back and one leg forward. Lean into the wall and bend your front leg while keeping your back leg straight. Deepen the bend until you feel a stretch through your back calf. Hold for 20-30 seconds and repeat 2-3 times on both sides.
- Plantar Fascia Stretch – From a seated position, rest your affected foot on the other knee. Gently grasp your toes and pull them towards you until your plantar fascia is stretched like a tight band across the bottom of your foot. Hold for 20-30 seconds and repeat 2-3 times.
- Physical Therapy – Physical Therapists are familiar with Plantar Fasciitis and can work alongside your Pedorthist to provide exercises specific to your body and condition.
- Massage the Area – Massage can relieve Plantar Fasciitis pain and reduce the likelihood of it becoming chronic. Try some of these techniques before getting out of bed in the morning to reduce the initial discomfort of those first few steps:
- Heel of the Hand – Use the heel of your hand to push down on the sole of your foot; start with light, small strokes, and then lengthen the strokes as you increase the pressure.
- Thumb Pulls – Use both thumbs to pull towards opposite sides of the sole of your foot for 1-2 minutes. Increase the pressure by using more bodyweight
- Thumb Pushes – Use both thumbs to move along the sole of your foot from heel to toe for 1-2 minutes. Try flexing your toes for added stimulation.
- Ball Massage – Sitting in a chair, place a small ball under your foot and gently roll back and forth for about a minute. Change your position and body weight to increase or decrease the pressure.
- Ice Massage – Similar to the ball massage, but use a frozen water bottle instead of a ball.
- Calf Massage – Your calf muscles impact your plantar fascia, so don’t forget to also massage your calves when using these techniques.
- Night Splints – Night splints essentially maintain a gentle stretch for your plantar fascia while you are sleeping. Your Pedorthist can assess whether or not they are the right choice for you and can recommend the brand and style that will best suit your particular needs.
- Extracorporeal Shock Wave Therapy (ESWT) – If your Plantar Fasciitis symptoms do not resolve with any of the above treatments, your health care provider may suggest ESWT. This type of therapy uses intense sound waves aimed at your heel to stimulate healing of the ligament. ESWT does not have a consistent record of success but can be worth a try with Plantar Fasciitis.
- Side Effects of ESWT – Side effects can include bruises, swelling, pain, and numbness.
Surgical Treatment for Plantar Fasciitis
Though rare, there are instances where surgical intervention may be considered an option for treating chronically debilitating Plantar Fasciitis. Like any invasive procedure, surgery for Plantar Fasciitis comes with inherent risks and is only considered if the pain is still severe after all other treatment options have been exhausted for a minimum of six months. Twenty-five percent of people who undergo surgical treatment for Plantar Fasciitis do not experience any improvement in their symptoms; the other seventy-five percent do report a decrease in pain. There are two main types of surgical intervention for Plantar Fasciitis.
- Gastrocnemius Recession – This procedure essentially lengthens the muscles and tendons at the back of the leg, which allows the heel to shift downward in a more natural position.
- Plantar Fascia Release (Endoscopic Plantar Fasciotomy–EPF) – This outpatient surgery takes only about 15-20 minutes to perform; a small cut is made in the plantar fascia to increase its flexibility and range of motion.
What are the best shoes for plantar fasciitis?
When it comes to treating and managing plantar fasciitis, the right shoe can make a big difference. The best shoes for plantar fasciitis are those that provide adequate arch support, cushioning, and stability. Look for shoes with a firm heel counter, a deep heel cup, and a rocker sole to help reduce the stress on the plantar fascia. Also, a good shoe for plantar fasciitis should have a flexible forefoot and a non-slip sole. Orthotic inserts can also be added to provide additional arch support. Athletic shoes such as running shoes or walking shoes are recommended for people with plantar fasciitis, as they provide the necessary support, cushioning and stability. You should avoid definately shoes with high heels or shoes that do not provide enough support for the foot. It is important to try the shoes on and walk around in them to make sure they are comfortable and provide the necessary support.
What Happens if You Don’t Treat Plantar Fasciitis
While Plantar Fasciitis can resolve on its own sometimes, it can be a long process. And it can also get worse before it gets better. So don’t ignore it! Even simple treatment options can be highly effective and can keep Plantar Fasciitis from becoming a chronic condition. If you suspect you may have Plantar Fasciitis, talk to your Pedorthist for an individualized treatment plan.
Conclusion
To conclude, Plantar Fasciitis is a common cause of heel pain that can range from mild to debilitating. Caused by stress to the plantar fascia ligament, it has a variety of symptoms, risk factors, and treatment options. If you are experiencing heel pain and think it might be Plantar Fasciitis, see your Canadian Certified Pedorthist. For more information or to find a Pedorthist near you, contact the Pedorthic Association of Canada.
FAQ
Is Plantar Fasciitis More Common in Males or Females?
Women are slightly more likely to suffer from Plantar Fasciitis than men. In addition, Plantar Fasciitis is common in pregnant women due to extra stress and pressure on the feet.
Do Children Get Plantar Fasciitis?
Though rare, Plantar Fasciitis can occur in people of all ages, including children. Children who are high-level athletes, obese, or who wear poorly fitting shoes would be at higher risk than the general population.
What Are the Symptoms of Plantar Fasciitis?
The main symptom of Plantar Fasciitis is heel pain, which can range from stiffness or a dull ache to stabbing pain that makes you limp. In bad cases, Plantar Fasciitis can severely impact your lifestyle and can even feel like it radiates far beyond your heel.
Pain from Plantar Fasciitis is typically the worst first thing in the morning or after a period of inactivity. Those first few steps after resting can be excruciating, but the pain usually subsides (at least partially) with gentle activity. If you exercise too vigorously or for too long, the pain will return. It can also be triggered by long periods of standing.
What’s the Difference Between Plantar Fasciitis and Heel Spurs?
Heel spurs are small bony calcifications that form on the calcaneus (heel bone). Though they are found in roughly 50% of people with Plantar Fasciitis, they are not usually painful. Heel spurs form as your body works to reduce stress caused by excessive pulling of the plantar fascia.
Are Heel Spurs the Cause or Result of Plantar Fasciitis?
It’s no longer thought that heel spurs cause Plantar Fasciitis or vice-versa. They are often associated with Plantar Fasciitis, but in such cases, the pain comes from inflammation of the plantar fascia, not from the heel spurs themselves. Plantar Fasciitis and heel spurs can also occur independently of one another.
Can Plantar Fasciitis Go Away on Its Own?
Yes. It can. However, it can take a long time to go away–sometimes years. The severity of your case along with your risk factors and lifestyle will impact how quickly you may heal. Ignoring Plantar Fasciitis is never a good idea. A Certified Pedorthist can put you on the right track to improving your Plantar Fasciitis as quickly as possible and taking preventative measures to keep it from flaring up again in the future.